Caring for Your Ultrasound Transducer: Top Cleaning and Disinfection Tips

Ultrasound imaging is a tool that is frequently performed by sonographers, doctors, nurses, and other medical professionals. With increasingly higher numbers of clinicians using ultrasound, it's more important than ever to ensure that everyone on your team knows how to care for their transducers properly.

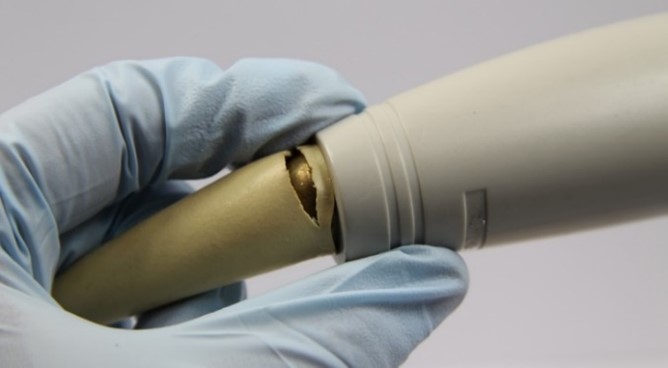
A significant issue can arise when transducers are not cared for appropriately. In fact, transducer misuse even has a hashtag on Twitter - #ProbeCrime. Some common #ProbeCrimes frequently documented include hanging transducers upside down, transporting or storing transducers with gel and/or body fluids on them, allowing transducer cords to drag on the ground, and storing transducers in inappropriate places. Damage to the transducer can occur in many ways, including to the transducer's cord, adaptor, face, and even its inner components.
Proper care and disinfection of transducers are both essential and beneficial; they can prolong the life of the transducer, ensure optimized imaging capabilities, and protect patient and clinician health. When medical equipment breaks down, there can be clinical implications, as well as negative effects on workflow and productivity. Hospitals and healthcare providers know that the performance of their equipment profoundly affects the quality of patient care. Between the high cost of service contracts (up to 10 percent of the system purchase price per year) 1 and the potential loss of revenue associated with decreased patient throughput, service issues can wreak havoc on capital budgets, leaving clinicians wondering what the best course of action is to safeguard their equipment. One of the most effective ways to prolong the life of ultrasound transducers is to properly clean, disinfect, store, and transport all transducers.
How To Protect Your Ultrasound Transducers
No matter what type of ultrasound transducer you might be using, when it comes to protecting and caring for your probe, there are a few crucial elements on which to focus. These include:

Cleaning: One of the most important things you can do when caring for your transducer is to ensure that it undergoes regular, thorough cleaning after each procedure. According to AIUM, 2 running the transducer under running water, while using a damp gauze pad or soft cloth with liquid soap to cleanse the device of any remaining organic material, can be critical in ensuring that your transducer remains infection-free. Also, remember to dry the transducer after cleaning, as residual water can potentially result in the fostering of additional bacteria on the transducer's surface.
High-Level Disinfection (HLD): Depending on what type of transducer you are using - or the type of procedure you are using it for - your transducer may be required to undergo high-level disinfection. The CDC defines high-level disinfection as the "complete elimination of all microorganisms in or on an instrument, except for a small number of bacterial spores."3 Typically utilized after a device that is classified by the Spaulding Classification as being "semi-critical" (i.e., any ultrasound transducer that contacts mucous membranes or non-intact skin) is handled during a medical procedure, HLD is used as a means of sanitizing the device of any and all potential contamination, and can be completed either manually (i.e. by-hand) using a commercially available germicidal soak, or automatically with an automated transducer reprocessor.
Even if your transducer is not classified as semi-critical, it may still require a specific method of cleaning or disinfection, according to the Spaulding Classification. After using a transducer for a procedure, always remember to consult the Spaulding Classification to see if it qualifies as either a "semi-critical device", a "non-critical" device (i.e., any device that comes into contact with intact skin), in which case low-level disinfection is usually required, or a "critical" device, (i.e. any device that comes into contact with the bloodstream or other sterile areas of the body), in which case full sterilization of the device is required. 3
Transport: Daily transport of ultrasound transducers can pose significant challenges to infection control and transducer safety for any department. According to ANSI/AAMI,4 "the type of container used [for probe transportation] depends on the items being transported. Bins with lids, enclosed or covered carts, rigid sterilization containers, and impermeable bags are among the types of containers that may be used." There are several specific steps you can take to help ensure the safe transportation of your transducers, including using a rigid container with a lid that secures the device in place and not bending the coil or shaft of the transducer while placing the device in the tray in such a way that results in kinking. No matter what type of transducer you are transporting, it's important to ensure safe and secure transport for your device.
Storage: Making sure that your ultrasound transducers are properly stored after use, particularly post high-level disinfection, is another important aspect in ensuring its care. Although seemingly simple, this can be much harder to accomplish effectively than one might initially think. The Joint Commission recommends that users store their transducers in a manner that will protect them from damage or contamination, such as hanging them vertically in a cabinet or storing them in a clean environment. 5
There are a variety of ways to store transducers to help safeguard them against damage or contamination, including checking that they are completely dry and also keeping disinfected transducers away from dirty probes while storing. Another way to ensure safe and secure storage is to utilize a transducer storage system that incorporates a fan and HEPA filtration, which can aid in the drying process and provide positive pressure to help to negate the threat of infection during storage. A recent study analyzed the effectiveness of these systems in reducing the presence of harmful pathogens on TEE probes when combined with longer clean storage hanging times, ultimately concluding that the risk of pathogenic bacteria growth on probe surfaces following storage in such systems is significantly lowered.
5 Ways to Keep Your Transducer Safe
- Consider an automated transducer disinfection system. Automated transducer disinfection systems offer an alternative to manual disinfection, providing a method of performing HLD that is faster, safer, and more efficient.
- Pick the right high-level disinfectant solution for your transducers. Not every high-level disinfectant is right for every transducer. Make sure you research the different types of disinfectant solutions, to determine the pros and cons, and then pick the one that is best for your specific transducer.
- Securely transport your transducers. Transportation of transducers post-procedure is often, unfortunately, a process that results in damaged or even broken transducers. Invest in a well-protected transportation tray or bag and take steps to ensure that the transport process itself is safe and secure.
- Store your transducers the right way. Properly storing your transducers post-procedure is a crucial component of making sure that they stay infection-free. Remember to store your transducers for the designated amount of time and consider utilizing a transducer storage system to help your transducers receive even greater security and filtration.
- Regularly clean your ultrasound transducer, as well as check for defects. All transducers require regular and thorough cleaning, even if they've barely been used. Make a habit of cleaning your transducer in its entirety, even those areas that are hard to reach, and while doing so, be diligent about inspecting the device for any holes, chips, or defects that might pose a risk to the device's integrity, as well as your patient's safety.
Explore CIVCO Medical Solutions
<For more than 35 years, CIVCO Medical Solutions has been committed to making image-guided procedures safer through the design, manufacturing, and marketing of medical products. Our products are trusted by physicians and clinicians in radiology, regional anesthesia, vascular access, men's and women's health, cardiology, infection control, sterile processing, and surgery, primarily focusing on the use of ultrasound. Our mission is clear: we seek to enable clinicians to provide safer outcomes by developing patient-focused products while delivering outstanding service and superior quality.
References:
- How to Evaluate an Equipment Service Contract (AORN, 2008 - https://www.aorn.org/outpatient-surgery/articles/outpatient-surgery-magazine/2001/november/how-to-evaluate-an-equipment-service-contract
- AIUM Official Statements 57. Guidelines for Cleaning and Preparing External- and Internal-Use Ultrasound Transducers and Equipment Between Patients as well as Safe Handling and Use of Ultrasound Coupling Gel https://www.aium.org/officialStatements/57
- A Rational Approach to Disinfection and Sterilization -= Guideline for Disinfection and Sterilization in Healthcare Facilities (2008) https://www.cdc.gov/infectioncontrol/guidelines/disinfection/rational-approach.html
- ANSI/AAMI 2013:ST58, "Chemical sterilization and high-level disinfection in health care facilities", 2013 (https://webstore.ansi.org/Standards/AAMI/ansiaamist582013r2018)
- The Joint Commission, High-Level Disinfection (HLD) and Sterilization Booster Pak (https://sdapic.org/wp-content/uploads/2015/12/TJC-HLD-BoosterPak-Dec-2015.pdf)








